Important Disclaimer: The information on this page is often historical and should not be used to guide surgical decisions.
| Sex
Re-assignment Surgery (SRS), or more accurately Gender Confirmation Surgery (GCS), for male-to-female transsexual women is well
covered on many Internet Websites and by other sources. Far less
information is available about castration, technically know as an
Orchiectomy or Orchidectomy in "British" English. However, a Bilateral Orchiectomy (removal of both testes) is a serious alternative to antiandrogen therapy for androgen suppression in preoperative transsexual women, and is now widely regarded as a useful precursor to SRS in many cases. Surgical ProcedureOrchiectomy is an operation for the surgical removal of the testes. The vast majority of the male hormone testosterone is produced in the testicles, so an orchiectomy is a very effective way of almost completely eliminating its masculinising effects on a body.
The testes are conveniently located external to the body cavity, they are relatively easy to remove and an orchiectomy is considered to be a quite minor operation. A small incision is made in the scrotum, the sac that contains the testicles. The testicles are detached from blood vessels and the vas deferens (the tube that carries sperm to the prostate before ejaculation) and removed, and the sac is sewn back up. That's it - it's a simple, cheap and low risk procedure by modern standards.
Orchiectomy can be performed as an outpatient procedure under local anaesthesia, or under general anaesthesia with an overnight stay in hospital.
|
|
|
Reasons that may lead a transsexual women to request a bilateral Orchiectomy include: eliminating male sexual urges; a desire to prevent further physical masculinisation; concern about liver damage due to prolonged use of anti-androgens; avoidance of testicular discomfort when wearing tight under-wear/swimwear; an inability to proceed with SRS for some reason.
Orchiectomy is particularly valuable for transsexual women who find they are intolerant to Cyproterone Acetate, whose unpleasant side effects can include: weight gain, fatigue, alteration of sleep patterns, mood swings, headaches, depression, hot and cold sweats, and intolerance to alcohol (particularly red wine on my experience!).
 An "aroused" penis a few months after an orchiectomy,  An "aroused" penis after an orchiectomy and several years taking female hormones. |
The effects of Orchiectomy include:
The hot flushes and fatigue are similar to those experienced by women during menopause. They are characterised by a sudden spread of warmth to the face, neck, and upper torso, usually followed by profuse sweating.
The fatigue is caused by decreased testosterone production and anemia - a deficiency of red blood cells. This results in a feeling of extreme tiredness that may not be alleviated by rest or sleep.
Overall there may be a change in temperament with docility, sluggishness and lethargy, as well as reduced energy, weight gain, and after several years reduced face and body hair.
Many of the above problems can be countered by taking oestrogen based HRT, but this will inevitably result in additional physical feminisation such as an ever shrinking penis, breast enlargement, fat deposits, and new problems such as cellulite.
There is also a long-term danger of osteoporosis, a loss of bone mineral density where the bones become thinner, more brittle, and at increased risk for breaking. It is the same condition experienced by women in menopause. Osteoporosis can be treated with oestrogen, calcium, and vitamin D. An exercise program with progressive weight-bearing activities will also help strengthen the bones, and help keep weight down.
The results of
the operation vary in their intensity with several factors, primarily on
the age of the man at the time. When a bilateral
orchiectomy is done before puberty, the results in terms of increased
physical feminisation and decreased masculinisation are much more
dramatic than when it is done after puberty. For example, the
voice remains high-pitched when the operation is performed before about
age 12, but does not change from the typical male low pitch when
performed after age 21.
 Advantages to the
Transsexual Woman
Advantages to the
Transsexual Woman[Please note that the following information is mostly taking from the Looking Glass website.]
A Bilateral Orchiectomy offers several unique advantages over antiandrogen or GnRH-agonist therapy for the transsexual woman:
Safety
The surgical procedure is simple and can be done under local
anaesthesia. After Orchiectomy, the patient is endocrinologically
equivalent to a post-operative subject and should take the appropriate
(lower) dosage of feminising hormones; there is no need for any further
antiandrogen therapy. This has clear safety advantages especially
in patients thought to be at elevated risk of thromboembolic
events. For long-term use (e.g. in patients who cannot afford SRS
for a considerable time, or for whom SRS is contraindicated by other
conditions), this is particularly significant.
Immediacy
It is generally impossible for a woman to obtain SRS without living
in role for at least a year. However this requirement does not apply to
an orchiectomy, which is not covered in the Harry
Benjamin Standards of Care.
 The brutal reality of the surgeons first cut for a transsexual woman's bilateral orchiectomy |
Minimal
Side
Effects
Some women report transient lethargy as their body adapts to the
loss of androgens, but the side effects associated with taking antiandrogens or GnRH agonists are
avoided.
Improved
Feminisation
In a post-Orchiectomy woman, feminising hormones can act
unopposed. This produces more complete and more rapid feminisation than
is normally achievable with antiandrogens.
No
Reversion
When feminising hormones are withdrawn prior to any surgery,
or for any other reason, the patient will not revert towards male
biochemistry or appearance. This is of enormous psychological
benefit in many patients.
Psychological
Benefits
Transsexual women report a feeling of progress or
achievement, of "asserting their true nature over a physical
deformity", and of looking 'less masculine' in the genital
area. This can produce a significant improvement in
emotional well-being.
Incidental
Health Benefits
It is claimed that a bilateral Orchiectomy protects against
coronary artery disease, cerebrovascular disease and effectively
increases the life span by an average of 5 years.
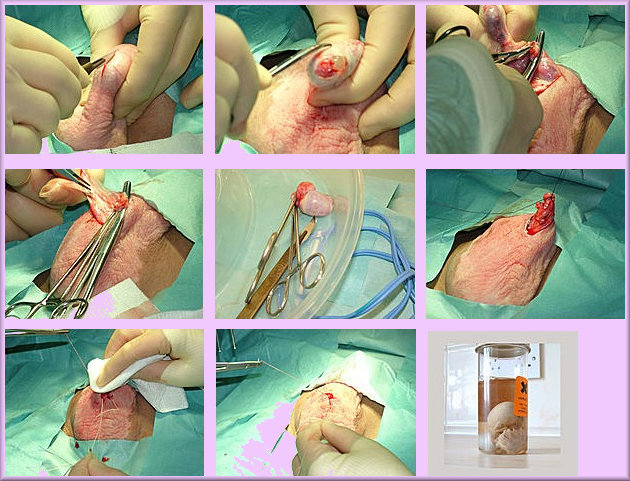
Photo's of Alison Faraday having her orchidectomy, age 22. The final
image is presumably
a joke! Alison sadly
died in a car crash in 2011, age just 28.
There are some disadvantages to having an Orchiectomy.
 Risk
Risk
Surgery, even a relatively simple procedure, carries risks related
to the anaesthesia and bleeding, and also possible post-operative
complications including abscess/infection and healing problems.
The following disadvantages also apply which can be very significant for the not completely committed transsexual woman who wishes to keep open the option of reverting to being male:
Irreversibility
Infertility
Orchiectomy will cause a complete and irreversible loss of sperm
production, with permanent sterility. Male sex drive and sexual
function can in principle be restored by administration of testosterone
should the woman decide to revert to a male role.
Conversely, long-term female hormone/antiandrogen therapy is also not
truly reversible.
Shrinkage of
Scrotal Tissue
If SRS is not performed for a considerable period after
Orchiectomy (e.g. 3 years or more), there is a risk of atrophy and
shrinkage of the scrotal tissue, reducing the amount of donor material
available for eventual SRS. This may or may not cause a problem,
depending on the patient's anatomy and the surgeon's technique.
However, again long-term hormone/antiandrogen use can also produce
significant atrophy of penile and scrotal tissue, and surgeons normally
recommend 'stretching exercises' to limit this effect; this method can
equally be applied to scrotal tissue after Orchiectomy.
If you are considering an orchiectomy as a preliminary to sex re-assignment surgery, then it's important to note that some popular surgeons are very reluctant to carry out SRS on patients who have already had an orchiectomy.
 A transwoman recovering from her orchiectomy after the wound dressing was removed. She was very happy with the procedure and had no complications. The skin browning is from the application of iodine. |
Seven of the group have now undergone SRS. The waiting time between Orchiectomy and SRS varied between 3 months and 34 months, with an average of 16.7 months. The study looked at whether Orchiectomy increased or decreased the need for SRS. Seven said that it made no difference, 5 said that it increased or confirmed their need for SRS, and in 2 patients it decreased their need for SRS.
Of the patients who subsequently underwent SRS none had surgical complications or complaints about vaginal depth as a result of Orchiectomy.
Of the 50% of
patients who had not yet had SRS, 3 had not yet changed gender role. Two
are currently on the waiting list for SRS, and one is waiting for NHS
funding. The other does not wish to have SRS.
To some women, one of the great advantages of Orchiectomy compared with SRS is the much lower cost.
 SRS
can cost anything from $8000 to over $20,000 for a top class surgeon
(and sadly, you often get what you pay for). In comparison, a
Bilateral Orchiectomy in the USA is available for as little as $1200
when done under local anaesthesia as a day case, going up to about $5000
with general anaesthesia and an overnight stay in hospital. In the
UK, Orchiectomy surgery is available privately for approximately £1500
($2200) when done under general anaesthesia with an overnight
stay.
SRS
can cost anything from $8000 to over $20,000 for a top class surgeon
(and sadly, you often get what you pay for). In comparison, a
Bilateral Orchiectomy in the USA is available for as little as $1200
when done under local anaesthesia as a day case, going up to about $5000
with general anaesthesia and an overnight stay in hospital. In the
UK, Orchiectomy surgery is available privately for approximately £1500
($2200) when done under general anaesthesia with an overnight
stay.
Orchiectomy
surgery is also very cost-effective in comparison with long term
androgen suppression treatment, whose costs can easily amount to $1000
or more a year, depending on the drugs being taken.
There are several "do-it-yourself methods for Orchiectomy. The following two methods are intended on farm animals but there are reports from hospital Accident and Emergency Departments of these being used by some men and transwomnen on themselves!
The very best that can be said about these methods is that they are very dangerous and DIY Orchiectomy is foolish in the extreme.
My friend Ellen Rugowski has generously provided the following account of her Orchiectomy procedure specifically for this page:
|
My Orchidechtomy by
Ellen Rugowski On July 7, 2001 at 8:50am, I underwent another step in my gender transition; I had an Orchidechtomy. This procedure, was done on an outpatient basis. My reasons for having an Ochidechtomy were threefold: 1.) The Gender program I am in (the Milwaukee Transgender Program in Milwaukee, Wisconsin) recommends (although it does not enforce), that if you haven't had SRS after 2 years of hormones, you either discontinue hormones (to lower the risk of clotting), or have an Orchidechtomy, and lower your hormone dosages (to lessen clotting risks). I have been on hormones for almost two years. 2.) Unfortunately, in spite of almost two years of hormonal usage, my testicles really never shrank. They were oversized to begin with, which made them hard to conceal. As I got further into transitioning, this became a matter of concern to me. I hated the bulge between my legs (and the testicles for that matter), and wanted it gone. 3.) I also
had my Orchidechtomy for economic reasons: I arrived at the Urologist's office for my Orchiectomy, at 8:20pm. While I was waiting to go into the surgical area for the Orchidechtomy, I talked with a pre-op friend of mine named Brenda, who was waiting for Crystal (also a pre-op MTF friend of mine), the patient before me, to finish with her Orchidechtomy. It is not recommended for patients, to drive themselves home after an Orchidechtomy, so Brenda was driving Crystal home, after her surgery was done. I was feeling quite nervous (like I used to feel when I was a competition runner; you're sure you're going to feel rotten after the whole affair is over with). At around 8:40am, Crystal came out to the waiting room. She looked a little pale, and had a sheen of sweat on her face. This made me even more nervous! The surgical nurse assisting the doctor took my blood pressure at this time, it was 150 over 100! I paid the doctor for the Orchidechtomy. The basic cost is 1100 dollars (780 pounds). Mine cost a bit more, due to the fact that it was discovered during my initial consultation appointment on May 31, that I had a varicose vein on one of my testicles, which would have to be tied off during the surgery, to prevent bleeding. At that time, I paid the doctor 300 dollars (212 pounds). I was also charged the basic fee mentioned above, which is what I paid on the day of my Orchidechtomy. So, my total cost, was 1400 dollars (990 pounds). I was then sent into the surgical room, told to take off my sandals, disrobe from the waist down, and lay down on the operating table. Several minutes later, the doctor arrived, told me to relax (I was pretty nervous at this time) and spread my legs. She then placed her surgical instrument kit between my spread legs. I was then given an injection of a nerve blocking type of local anesthetic, at two points on either side of, and roughly at the level of the penis. The doctor then waited about three or four minutes for the anesthetic to take effect, and the surgery began. The surgical method used, involved making two incisions, one on each side of the penis, in the upper part of the scrotal sac. Each testicle, was removed, one at a time. The first testicle removed, was the left one (as viewed from looking at me head on). An incision was made, and the doctor used her fingers to create a passageway (called a blunt dissection- this is the same way, the vaginal opening is started, during SRS), that the testicle could be pushed through. The doctor was surprised to discover that I had three very large varicose veins on the left testicle. These had not been detected during the initial consultation appointment. They were quite large, and had to be tied off to prevent bleeding. Once the varicose veins were tied off, and the ligaments holding the left testicle in the scrotal sac were cut, the testicle was pushed out of the scrotal sac. It was only attached to the spermatic cord. The testicle was then pulled on, until the spermatic cord was taut, and the spermatic cord was cut (the tautness in the cord, caused the stump of the cut cord, to snap back into the abdominal cavity, where it wouldn't protrude next to the skin, and be subject to painful feeling bumps). When the spermatic cord was pulled taut, I could feel my upper groin area tense up. The incision was then closed up, and the doctor proceeded to remove the right testicle (as viewed from head on). The procedure to remove the right testicle, was the same as the procedure to remove the left testicle. This was the testicle, that the doctor had discovered the varicose vein on, during my consultation appointment on May 31. When the incision was made, this testicle was found to have two additional varicose veins on it, for a total of three varicose veins! All of them were quite large according to the doctor. As on the left testicle, the veins had to be tied off. The right testicle was then removed (with me once again feeling a pulling sensation in my upper groin area, when spermatic cord was pulled taut). At this time, the doctor remarked that she was surprised that I had virtually no shrinkage in my testicles, in spite of almost 2 years of hormonal use. The incision was then closed up, the sutures were bandaged, I was helped to get dressed, and I went out to the waiting room to wait for my ride. While I was waiting for my ride, my blood pressure was taken, it was back to normal. My friend Blake (a FTM), arrived at around 10 am to pick me up (he went to do some things, while I was having my surgery), and we left. To celebrate, Blake treated me to brunch. We then went to Blake's house, where I spent the next several hours waiting for Ashley (a MTF Intersex woman) to arrive, and drive me back home (an hour and a half north of Milwaukee, in the Manitowoc area). When Ashley, arrived, her Blake, and I went out for supper. Ashley and I then made the 85 mile drive home. During the time after my surgery was done, until I arrived home, I took it very easy. I moved, and sat in a reclined manner, to avoid pulling on my stitches. The pain wasn't much of a problem, just a generalized ache in the groin area. There was some swelling in the groin area, which I controlled by applying cold packs to the surgical areas. I began to take antibiotics, and Vicodin ( a pain medication I was prescribed). I also started to swab an Iodine solution on the surgical sites. This had to be done three times a day to help prevent a infection on the surgical site. I also changed the bandages, when I applied iodine. I didn't have to be back to work, until July 10. So I spent the following Sunday and Monday, taking it easy. I mainly just laid out in a lawn chair on my apartment balcony reading, and napping, when I wasn't swabbing Iodine on my sutures, and changing bandages. I wasn't allowed to wash up (other than a sponge bath), until Monday July 9. On Monday I could wash up, but no baths were allowed, only showers, until I was cleared by the doctor at my post-op follow-up appointment on July 24. I also had to be careful to minimize the amount of soaking I did to the surgical suture areas, when I showered. I went back to work on Tuesday July 10. I took it easy at work for the next week and a half. I was a little sore in the groin area. The surgical area basically ached like a bad groin pull, and did this for about the next week or so. By about a week post-op, the pain had went down enough, that I discontinued use of the Vicodin. I was also able to start going for long walks, in order to get some exercise (I was not allowed to start running again, until the doctor OKed it ). I was also able to stop using gauze dressings (everything was healing well), and just use a few Band Aids over the suture areas, to protect things. On July 24, I went for my post-op examination. The doctor who performed the surgery told me that everything had healed up very well, and I was cleared to start running, taking baths again, and normal activities in general. As of July 26, I'm doing well. There are still some infrequent minor pains in the groin muscles near the surgical sites. These are easily handled by taking a couple of Ibuprofen. Everyday, these pains occur less often. Do I think it was worth it to have an Orchidechtomy. Definitely. The varicose veins on my testicles, would have made them a medical problem in years to come. Also, it's nice not to have that ridiculously large bulge I used to have between my legs. My electrolysis costs have already started to fall to about 50 percent of what they used to be, due to the lack of testosterone in my system, which gives me more money to use for other things (like SRS). May you be able to pursue those things you find worthwhile in life. Hugs, |
Sadly Ellen passed away in 2020, age just 56.
(c) 2000 - 2024 Annie Richards
Please send any comments, feedback or additions to:
Last updated: 30 June, 2002