
[Part 1]

Notes:
The primary purpose of the female human breast is to provide sustenance and nourishment to a baby, with a secondary purpose of attracting a high-quality mate to father the child. Breastfeeding is usually strongly recommended by doctors; it is by far and away the best and most convenient way to feed a baby. Not only will the baby be healthier, but it also helps the new mother lose weight more easily. Calories are burned during milk production; indeed some of the weight gained by a woman during pregnancy is intended to be used during lactation. Breastfeeding also releases a hormone in the woman's body that acts as a natural tranquillizer, filling the mother with a sense of calm and well-being while she is breastfeeding. No authoritative medical studies seem to have been conducted on the maternal desires and instincts of transwomen. But it seems safe to claim that a substantial proportion of at least younger transwomen would like to be a mother and breastfeed a baby. Nursing and Transwomen While almost all transsexual women proudly regard their breasts as an important sign of their femininity and womanhood, only a few really consider their primary biological purpose. Nevertheless a few transwoman were seeking to induce lactation as far back as the late 1950's, albeit with very modest success. In the years since there has been huge medical advances. The breasts of a young transwoman - particularly if they started hormones as a young teenager - are often medically indistinguishable from those of a cis-female, and are just as capable of lacation. In 2005 an English newspaper published a story about a young woman breastfeeding her baby in a restaurant, she was asked to leave and wasn't happy about that. Not really headline material, but readers then discovered that the woman in question was a male-to-female transsexual. As a 'husband', she had begun female hormone treatment at about the same time as his/her wife had become pregnant. After the baby's birth, the transwoman had acupuncture to help kick-in her own milk production and was sharing nursing duties with her former wife.
Since then an increasing number of transwomen have realised from articles (including this website) that is possible for them to breastfeed. Statements by anti-transwomen campaigners such as Milli Hill's "Male people, however they identify or describe themselves, cannot breastfeed” are factually incorrect. In September 2022 the online magazine INSIDER published a contraversal article desrcibing how Some Parents Are Breastfeeding Without Pregnancy or Giving Birth. Another example is Mika Minio-Paluello, who identifies as a transgender woman and a lesbian, although still pre-GCS. In 2023 she published on Twitter a photo of her breastfeeding a baby born by her partner, hinting that IVF had been used. She had taken hormones and drugs to enable lacation and helped breastfeed the baby for a few weeks before sadly getting a cancer diagnosis that stopped this. The story was picked up by a UK television channel and she featured in a news item, causing considerable controversy about the ethics of a "man" breastfeeding. She was even reported to the National Society for the Prevention of Cruelty to Children (NSPCC), who quickly concluded that there was no risk to the child. Physical Requirements The breasts of a transsexual woman are quite capable of producing milk ("lactation") given the following circumstances:
Motivation Inducing lactation is not easy; it will often take a lot of time and a lot of effort over a long period. The necessary motivation is essential, or failure is almost inevitable.
Whilst quite such a high success rate cannot be achieved with male-to-female transsexual women, there's no doubt that given a high degree of motivation combined with medication, support, and encouragement; lactation induction can often be successful in transsexual women. Breast Augmentation A majority of transsexual women have had breast augmentation (implants), but the chances are good that the implants in themselves will not prevent lactation. Studies show that only about 10% of genetic XX woman with implants are unable to breast feed due to damage to their breasts caused by the implants. However, unfortunately many TS women have small and underdeveloped (hypoplastic) breasts prior to breast augmentation surgery. Although breast augmentation will greatly improve the external appearance of such breasts, even giving the impression of fully developed breasts, it does not solve the underlying milk supply problem due to insufficient internal development, and it will thus still be difficult for the woman to produce milk and nurse.
With a breast that has been surgically enlarged with implants, the nipple may be more or less sensitive than normal. If the nerves around the areola were not cut or damaged during the surgery then it should still be possible to nurse fully or partially. Nerves are vital to breastfeeding since they trigger the brain to release prolactin and oxytocin, two hormones that affect milk production. The chances of breastfeeding also improve if the milk duct system is intact. It's impossible to know the full extent of damage — if any — until a woman tries to make and express milk. Once lactation starts, implants may also cause exaggerated breast engorgement with more intense than normal pain, fever, and chills. The likelihood that implants cause serious lactation and milk production problems depends directly upon the kind of surgery had. Incisions that were made under the fold of the breast (inframammary) or through the armpit (transaxillary) shouldn't cause any trouble. However, the popular periareolar method involving an incision around the areola has greater risk of problems. After millions of breast augmentation procedures using silicone implants, there is no evidence that the silicone leaks into breast milk, and even if it did there is no evidence that it would then harm the baby. For example, a silicone-based medication, Simethicone, is used to treat a baby's stomach gas. Breast DevelopmentIn order to be able to produce milk internally the breast must have certain structures in place, but fortunately these are present at birth in every human, whether genetically male or female. It's also worth noting that highly visible factors such as breast size and areola diameter that are often of great importance to transsexual women in fact have relatively little effect on the breasts potential ability to lactate and the quantity and quality of the milk that will be produced. Whatever the size of her breasts, a M2F transsexual woman can still potentially breastfeed if the internal structures are in place and undamaged.
At birth the rudiments of the functional mammary gland are in place: the nipple and areola are formed along with a rudimentary system of mammary ducts extending into a small fat pad on the chest wall. The mammary gland remains a rudimentary system of small ducts until puberty when the advent of oestrogen secretion by the ovaries brings about the first stage of the four stages of mammary development: mammogenesis, lactogenesis, lactation and involution. Mammogenesis commences at puberty with the onset of oestrogen secretion by the ovaries, usually between the ages of 10 and 12 in the girl. Oestrogen causes enlargement of the mammary fat pad, one of the most oestrogen-sensitive tissues in the human body, as well as lengthening and branching of the mammary ducts. About 40% of male children also initiate mammary development during puberty due to the tendency of the testis to secrete significant quantities of oestrogens in early phases of its development. As testosterone secretion increases this function is lost. Oestrogen stimulates breast growth by acting on the mammary tissue. With the onset of the menstrual cycle the presence of progesterone stimulates the partial development of mammary alveoli, so that by the age of 20 the mammary gland in the woman who has not been pregnant consists of a fat pad through which course 10 to 15 long branching ducts, terminating in grape-like bunches of mammary alveoli. In the absence of pregnancy the gland maintains this structure until menopause. Mammogenesis is completed during pregnancy, with the gland becoming able to secrete milk sometime after mid-pregnancy. Lactogenesis (referred to as the time when the milk "comes in") starts about 40 hours after birth of the infant and is largely complete within five days. When nursing has ceased the gland undergoes partial involution, losing many of its milk producing cells and structures, a process which is only completed after menopause.
Breast
Development in the Transsexual Woman The amount of hormone induced breast development achieved in the genetically XY male transsexual woman is very age dependent. Young boy-to-girls who start female treatment during their normal puberty years (i.e. about age 12-16) are likely to reach near normal breast development. But unfortunately the amount of development that can be expected rapidly tails off as the age of the commencement of hormone increases, and older transsexual women will commonly suffer from underdeveloped (hypoplastic) breasts. Breast development
is categorised by the "Tanner Stages" scale which goes from I to V.
It can again be emphasized that there is really NO minimum degree of
breast development in order to be able to lactate; there are well
documented instances of even men with minimal Tanner I breasts producing
some milk and breastfeeding without using hormones.
Breast Development During Pregnancy It is necessary to understand how the human breast develops and prepares for milk production during a woman's pregnancy. Mammogenesis is completed during pregnancy - indeed pregnancy is the period of greatest mammary growth. Extensive lobular and alveolar development occurs only during pregnancy, also milk secretory cells only develop during pregnancy, therefore this period is extremely important in determining the number of secretory cells in the lactating gland and the subsequent production of milk. Mammary growth (of the mother) accelerates throughout pregnancy and is fastest during the later stages of pregnancy, which coincides with the most rapid period of foetal growth.
Breast
Structure of a Pregnant Woman
But perhaps even more remarkable than this visible transformation are the extensive changes taking place inside her breasts, primarily under the stimulation of high levels of oestrogen and progesterone, combined with the rising levels of prolactin from the pituitary and human placental lactogen (HPL) from the placenta.
Nestled amid the breasts fat cells and glandular tissue is an intricate network of channels or canals called milk ducts. The additional hormones released during pregnancy cause the cells of the mammary fat pad to diminish in size and their place is taken by the developing ducts and alveoli. 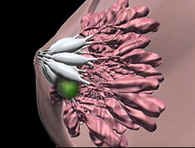 During
the first three months of pregnancy the milk ducts increase in number and
size; the ducts starting to branch off into smaller canals near the chest
wall called ductules. During the mid-three months a cluster of small,
grapelike, sacs called alveoli appear at the end of each ductule. A
cluster of alveoli is called a lobule; a cluster of lobules is called a
lobe. Each breast contains between 15 and 20 lobes, with one milk duct
for every lobe. During the last three months of pregnancy the alveoli
grow and mature. During
the first three months of pregnancy the milk ducts increase in number and
size; the ducts starting to branch off into smaller canals near the chest
wall called ductules. During the mid-three months a cluster of small,
grapelike, sacs called alveoli appear at the end of each ductule. A
cluster of alveoli is called a lobule; a cluster of lobules is called a
lobe. Each breast contains between 15 and 20 lobes, with one milk duct
for every lobe. During the last three months of pregnancy the alveoli
grow and mature.Milk is produced inside the alveoli, which are surrounded by tiny muscles that squeeze the glands and push milk out into the ductules. Those ductules lead to a bigger duct that widens into a milk pool or milk sinus directly beneath the areola. Milk pools (also known as sinus) act as reservoirs that hold milk until a baby suckles it through tiny openings in the nipple. Essentially the 15 or 20 milk ducts act as individual straws that all end at the tip of the nipple and deliver milk into a baby's mouth. The mammary gland becomes able to secrete milk sometime after mid-pregnancy, and begins to produce small amounts of a protein- and fat-rich secretion sometimes referred to as precolostrum. It seems likely that mammary development continues through the duration of pregnancy since milk secretion by mothers of premature infants often appears to be diminished. The onset of copious milk secretion (or lactogenesis) is held in check by the high levels of circulating progesterone until after childbirth.
Differentiation of the breast to its mature status occurs by the third month of pregnancy, although it will take about 6 months for the breast system to fully develop and become functional for lactation. Indeed, mammary growth will continue right up to birth, and even after if nursing. In a pregnant woman, by time the baby is born, glandular tissue has replaced most of the fat cells and accounts for the much-enlarged breast. The increase in size varies greatly with the individual, ranging from zero to 800 cc of volume (and 1½ lb of weight!) per breast; the average being about 400 cc. It is normal for women to increase by one or two cup sizes during pregnancy, although this will decline (sometimes dramatically) after the cessation of lactation. Oestrogen and Progesterone Optimal mammary growth requires both oestrogen and progesterone hormones.
Together, these result in growth of the lobular and alveolar system.
Both hormones are elevated during pregnancy, which is why there is no
such "lobuloalveolar" growth during a woman's oestrus (fertility) cycle,
when only one of these hormones is elevated at a time.
Progesterone is elevated throughout gestation (required for maintenance
of pregnancy), while oestrogen is particularly elevated during the
second half of gestation. Consequently, most of the mammary growth
during the first half of gestation is mainly ductal growth and lobular
formation. In the second half of gestation, ductal growth
continues, but most growth is lobuloalveolar.
During pregnancy, the mammary tissue has oestrogen receptors and progesterone receptors. During lactation the mammary gland has oestrogen receptors, but not progesterone receptors. Other hormones As well as the oestrogen and progesterone hormones well known to transsexual women, there are several other hormones important to breast development and milk production. Indeed, mammary development in the pregnant woman takes place under the influence of an extraordinarily complex mix of hormones, including:- prolactin, human placental lactogen, estradiol (a type of oestrogen), progesterone, insulin, cortisol, growth hormone, thyroid hormones ... Prolactin is a protein hormone secreted from the anterior pituitary gland, as well as assisting in breast development; it stimulates and controls the actual production of milk. In a pregnant woman, the placenta produces an important hormone called Human Placental Lactogen (HPL) which adjusts the maternal metabolism. One of its functions is similar to prolactin, i.e. stimulation of milk production by the mammary glands. HPL seems to work with oestrogen and progesterone to increase the number of alveoli in mammary glands and also plays a role in making the alveoli functional (capable of producing milk). It's thought that the level of HPL hormone activity in the maternal blood regulates the extent of mammary development during late pregnancy. HPL also causes the secretion of a form of milk called colostrum from about the fifth month of pregnancy. Yet another, and apparently unimportant, hormone is secreted by the pituitary gland of a pregnant woman, Melanocyte Stimulating Hormone (MSH). Its only known effect is to stimulate the skin to produce pigmentation, causing the aeroli to enlarge and darken.
Lactogenesis Lactogenesis is associated with an abrupt increase in milk volume secretion, which goes from a mean of about 50 ml per day on day 2 of lactation to about 500 ml per day on day 4. After this time there is a gradual volume increase to about 850 ml/day by three months postpartum. There are also profound changes in milk composition during the early post childbirth period as the production of milk products comes into high gear. By 10 days after childbirth the milk has assumed the composition characteristic of mature milk. There are minor composition changes that continue throughout lactation. Full lactation, or the secretion of mature milk, continues as long as the demand is there, up to three to four years for infants in some cultures. Three factors are necessary for successful lactogenesis: a developed mammary gland, continued high plasma prolactin levels, and a fall in progesterone and oestrogen levels that otherwise inhibit lactation - it can therefore be partially inhibited by high doses of oestrogen. It is important to note that the milk "comes in" at the same rate whether the infant suckles during the first 48 hours or not. Thus the onset of milk secretion depends, not on milk removal from the breast, but on the changes in hormonal status associated with child birth. However, continued milk secretion depends on milk removal from the breast, the involutional process sets in after only 3 to 4 days if breast-feeding is not initiated.
Breast Stimulation in the Transsexual WomanHormonal Stimulation Lacking the hormone producing ovaries and placenta present in a pregnant woman, the transsexual woman attempting to induce lactation must take oestrogen by some artificial means (oral, injection, patches, etc.). The oestrogen is then abruptly withdrawn to mimic the rapid hormonal changes following delivery.
If only a minimal degree of lactation is being attempted then the high oestrogen regimen may be as short as two weeks. But if full lactation is desired, then the transsexual woman must try to induce all the necessary developmental changes in her breasts by simulating a full period pregnancy by taking high doses of oestrogen and progesterone hormones for a period of at least six months (probably not coincidently, a premature baby born after the 28th week or sixth month of pregnancy is "viable" and will often survive, and will thus require feeding). This sustained hormone treatment may stimulate her breast in to developing and preparing for lactation, but unfortunately transsexual women with underdeveloped hypoplastic breasts are unlikely to succeed in this endeavour as their breasts will fail to respond to the additional hormones.
Assuming that the hormones have an effect, the period of the most visible breast growth is often during the first eight weeks of treatment. This enlargement is potentially just temporary as it's primarily due to engorgement of the blood vessels, enabling increased circulation to the breasts. Thereafter, oestrogen hormones stimulate cell mitosis and growth of the ductal system, the development and differentiation of the glandular tissue (lobules and alveoli) is dependent on progesterone, whilst breast fat accretion seems to require both. Regarding other hormones found in pregnant woman:
Mechanical Stimulation Most genetic women and some men can induce lactation to some extent with only mechanical stimulation. This consists of breast massage, nipple manipulation, and sucking - the later either by a baby or by expressing using a good quality electric breast pump with a double pump kit. Realistically expression by hand, or even with a hand pump, is simply not a practical alternative to an electric double breast pump given the frequent and prolonged sucking required on each breast. A possible expressing regime: Begin by expressing each breast for about five minutes, three times a day. Increase the length of the pumping session as you become more comfortable, until you are expressing for a total of about 15 to 20 minutes on each breast every two to three hours during the day. Expressing both breasts simultaneously by double-pumping obviously saves a lot of time every day by this point! You must include nighttime pumping sessions, allowing just one long 4-5 hours period of sleep. Constant expressing will soon get to become hard work, when after a week you still haven't seen any milk at all, try not to become discouraged or concerned, unfortunately it may well take four to six weeks for the breasts to begin producing milk this way. Some dedicated women have reported only finally achieving some success after two or three months pumping!
To pump effectively and increase milk supply it is essential to relax and stimulate as much as possible the milk let-down response crucial to milk expression. Suitable mental or environmental stimuli such as baby photo's, imagining yourself breastfeeding, direct sucking stimulation of the nipples and immediately surrounding tissue, playing a tape of the cries of a hungry baby, ... etc, are essential aids to milk production. And a partner can greatly assist with sexually arousing mental stimulation and manual manipulation of the woman's body before, and even during, her expression period.
Expression Routine It is essential to establish a routine to both start and then maintain lactation. For example, begin by expressing each breast for about five minutes, three times a day. Increase the length of the pumping session as you become more comfortable, until you are expressing for a total of about 15 to 20 minutes on each breast every two to three hours during the day. Expressing both breasts simultaneously by double-pumping obviously saves a lot of time every day by this point! You must include nighttime pumping sessions, allowing just one long 4-5 hours period of sleep. Here are some tips to help both manual and mechanical expression:
Achieving Milk Production in the Transsexual Woman
Lactogenesis At this
point mechanical breast stimulation, particularly sucking (with
a breast pump or by a baby) should be started and an oxytocin
nasal spray used to stimulate milk release. If not already
begun a course of a prolactin enhancing drug
such as domperidone (brand name Motilium) is highly
recommended to help milk production. [Although the US
Federal Drug Administration
warns against using the anti-nausea drug for this purpose.]
Success is not guaranteed, but some milk production can be expected in a
majority of cases. Milk production typically begins between 1-4 weeks
after initiating stimulation using prolactin enhancing drugs, although it
can be as little as 2-3 days if hormones were taken and were effective, or
as long as 4-6 weeks if relying purely on mechanical stimulation. One
study of induced lactation using enhancing medications describes the onset
of milk production being between 5-13 days. At first, the woman may
see only drops. During the time that milk production is building,
women may notice changes in the colour of the nipples and areolar tissue.
Breasts may become tender and fuller. Some women report increased
thirst, and changes in their menstrual cycle or libido.
As the body readies itself for lactation, it pumps extra blood into the
alveoli, making the breasts firm and full. Swollen blood vessels,
combined with an abundance of milk, may make the breasts temporarily painful
and engorged, but nursing or expressing frequently in the first few days
will help relieve any discomfort.
Milk Release When oxytocin reaches the breast it causes the tiny muscles
around the milk-filled alveoli to contract and squeeze.
The milk is emptied into the ducts, which transport it to the
milk pools just below the areola. When s/he suckles, the
nursing infant presses the milk from the pools into his mouth,
both manual and mechanical expression techniques can simulate
this to a reasonable degree.
A benefit of oxytocin is that it the nursing woman may feel
calm, satisfied, and even joyful as she nurses or expresses.
Maintaining Lactation The volume of milk produced is primarily a function of
demand and is unaffected by maternal factors such as nutrition or age.
Not a lot of milk will be produced unless suckling (natural or
artificial) is frequent and consistent, the milk itself contains an
inhibitor of milk production that builds up if the milk remains in the
mammary gland for a prolonged period of time. Adequate milk
removal from the breast is absolutely necessary for continued milk
production.
|
Part
2 of "Lactation and the
Transsexual Woman"...
![]()
Last updated: 28 August, 2024